
اهدای زندگی Life Donation
به نام خدا، مطالبی راجع به اهدای عضو-اهدای سلولهای بنیادی-اهدای خون-اهدای پلاکت-اهدای پلاسما با همکاری کانون اهدای زندگی دانشگاه بناب--- آدرس صفحه اینستاگرام: ehda.zendeghi@
اهدای زندگی Life Donation
به نام خدا، مطالبی راجع به اهدای عضو-اهدای سلولهای بنیادی-اهدای خون-اهدای پلاکت-اهدای پلاسما با همکاری کانون اهدای زندگی دانشگاه بناب--- آدرس صفحه اینستاگرام: ehda.zendeghi@Difference between brain death and coma: organ donation for brain death person
Brain death and coma are scientifically two completely different processes!
It is usually wrongly assumed that a brain-dead person has a chance of recovery, such as a person who has been in a coma. If you've heard that a person has suffered brain death and then recovered, it hasn't actually been brain death. Patients who have recovered are in fact in a deep coma, and after returning from a coma, their relatives or sometimes even some doctors and nurses who do not have enough information about the difference between brain death and coma have made such a misconception!
Therefore, sometimes relatives of a brain dead person mistakenly assume that he has a chance of recovery and return, so they do not consent to organ donation in the hope of recovery.
In a coma, there is a chance for some patients to recover, while brain death is, in medical terms, absolute death, and the person will never alive.
In brain death, the patient's recovery is impossible and his death within a few days is inevitable. Therefore, the opportunity to donate a brain-dead person's organ is limited to a few days!
Coma recognition
Cortical cells are highly sensitive to hypoxia, so when blood flow to these cells is stopped, they quickly become seriously and sometimes irreversibly damaged. In this case, the person quickly loses consciousness and, depending on the extent of damage to the cerebral cortex, his reactions to environmental stimuli are reduced. However, there is still the possibility of improving the condition and returning the consciousness of the disease that has gone into a coma.
Recognizing brain death
Brain death is the cessation of all brain activity and brainstem at the same time. a person with brain death is actually a person who, due to extensive brain damage, has been unable to communicate with his surroundings, cannot speak, does not see, does not respond to painful stimulations. A person with brain death is also unable to breathe spontaneously. Although he has a heartbeat, he has no recordable waves when we record his brain waves. His heart rate continues with the help of a ventilator and maintenance measures to keep donated organs in optimal conditions for transplantation. Brain death in medical science is absolute death and this person will never come back to life.
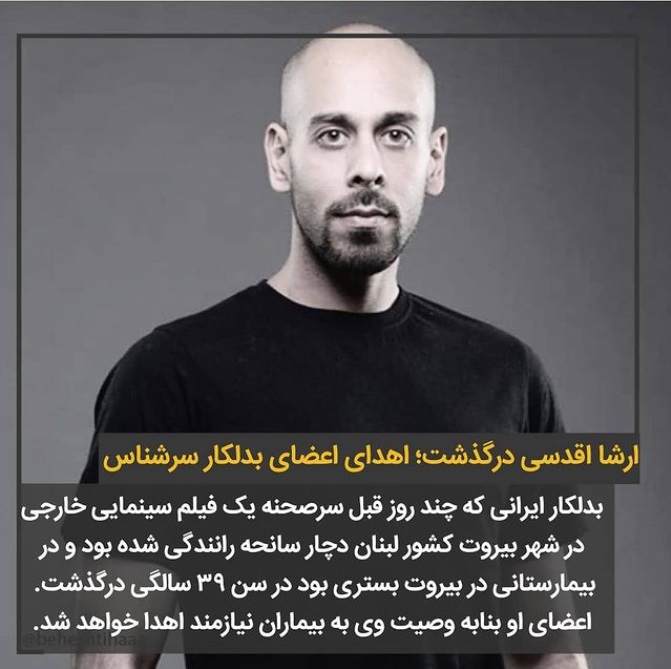
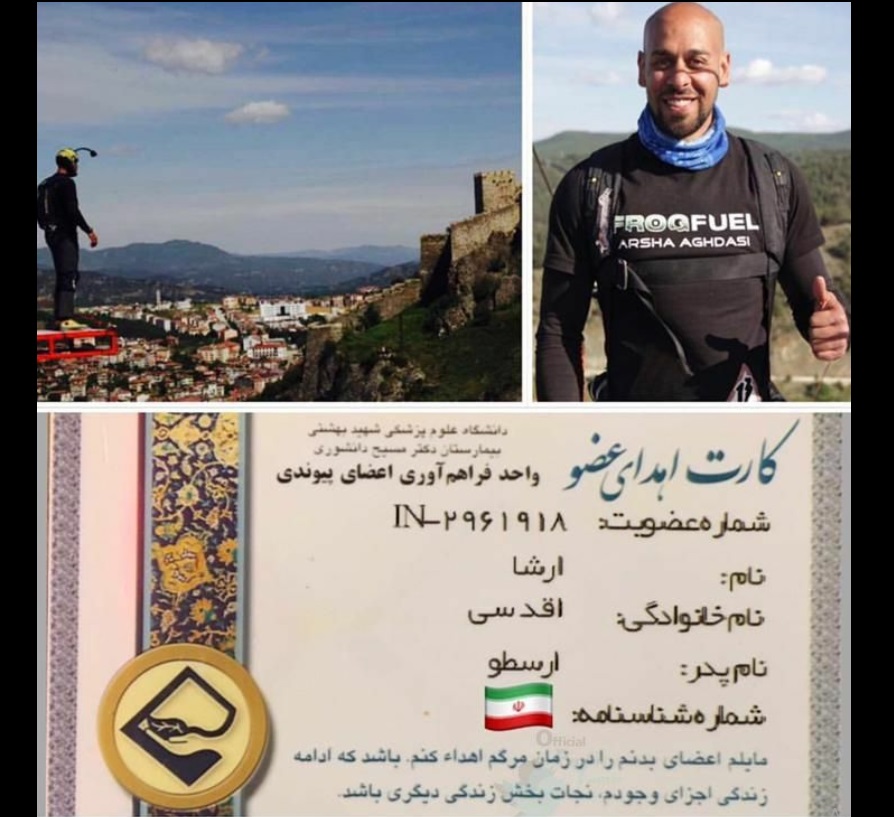
اندیشه والای زنده یاد ارشا اقدسی در خصوص اهدای عضو
اندیشه والای زنده یاد ارشا اقدسی در خصوص اهدای عضو، حاکی از قلب مهربان و روح بزرگ ایشان بود. روحش شاد و یادش گرامی
Donation card of the presenter of "Khandvaneh", Rambod Javan
Rambod Javan Tabrizi volunteered for organ donation in a humanitarian practice (Date of this news : 2017 January 8).
Young Journalists Club: "Organ Donatin, Life Donation". You must have heard this slogan a lot. It is both bitter and soothing. It is bitter for a mother who does not want to believe that her child's life's office in this world is closed, and at the same time the sound of her beating in another body can be soothing. Rambod Javan Tabrizi, the famous presenter of Khandvaneh program, was among those who joined the group of registered donors and shared a photo of his donation card on his instagram page.
"I would like to donate my organs and tissues at the time of my death, so that the continuation of my life will save another life."

Persian page link : https://ehda-zendeghi.blogsky.com
Translator : Javad Eynaki Maleki
Organ donation after brain death or cardiac death (typical death)
With the consent of the parents, all those who have suffered from brain death or cardiac death (normal death) can have their organs removed and transplanted into patients. All over the world, a few decades ago, brain death was considered equivalent to definite death, and in our country, according to the law (approved in 1379), brain death is equivalent to death. According to the same law, organs are allowed to be removed from cases of brain death as well as cardiac death with the consent of the family and its transplantation.
Organ donation after brain death:
The main human organs such as the heart, lungs, liver, kidney ... due to having the main blood vessels are destroyed as soon as they die. Therefore, these organs can only be removed from cases of brain death, and after removal, they can be stored for a short time and must be transplanted immediately. The donor should not have AIDS, hepatitis or cancer and should not be older than 60 years.
Organ donation after cardiac death:
Tissues such as bones, heart valves, tendons, corneas, etc. live longer and can be removed after normal death (cardiac death) and can be stored for years. Therefore, in cases of death (cardiac death), if the person does not have an infectious disease and timely information and consent is given, the tissue can be removed. The donor should not have AIDS, hepatitis or cancer and should not be older than 60 years.
----------------------------------------------------------------------------------------
Difference between brain death and coma:
Brain death is a state that the brain goes away and dies, but because the spinal cord is alive, the rest of the members (such as the heart) remain alive for a few days; In this case, the person's breathing is discontinued and there is no medical reflection of the individual's improvement or alive, and as soon as the devices are disconnected and the person dies, and with the device and medical care, there are only a few days of "vegetative state" for the individual.
Brain death differs with anesthesia or coma, and most of the accidents occur. To confirm brain death in Iran, they will keep watching 24 hours, and after a variety of experiments and approval of the six specialist appointed by the Minister and Forensic Medicine, and the work of transplantation should be done only in government universities.
Transplant recipients:
Transplant recipients are placed on the waiting list based on blood group, intensity of need and waiting time, and at the same time as the family consent of the deceased for organ donation, a number of transplant recipients will be examined in terms of size and weight and tissue matching tests to make the organ the most suitable person.
Transplant cost:
For a member or tissue, there is no way to pay a donor or receive a recipient, but it is costing for surgical procedures and member maintenance and experiments that are covered by insurance, and the government is paying most costs.
In the operation of organ harvesting from the deceased, the body is not mutated and replaced with the harvested prosthetic organ so that the shape of the body does not change.
Having a member card donor and written will is not enough! Family satisfaction is required:
It is imperative that even if the family consent, in the event of membership in this plan or written will, fails to prevent this. So, in order to ensure that this heart desire is made, keep your relatives from having a donated card and this benevolent decision.
Persian page link : https://ehda-zendeghi.blogsky.com
Translator : Javad Eynaki Maleki
July 31:National blood donation day
A blood donation occurs when a person voluntarily has blood drawn and used for transfusions and/or made into biopharmaceutical medications by a process called fractionation (separation of whole blood components). Donation may be of whole blood, or of specific components directly (apheresis). Blood banks often participate in the collection process as well as the procedures that follow it.
Today in the developed world, most blood donors are unpaid volunteers who donate blood for a community supply. In some countries, established supplies are limited and donors usually give blood when family or friends need a transfusion (directed donation). Many donors donate for several reasons, such as a form of charity, general awareness regarding the demand for blood, increased confidence in oneself, helping a personal friend or relative, and social pressure. Despite the many reasons that people donate, not enough potential donors actively donate. However, this is reversed during disasters when blood donations increase, often creating an excess supply that will have to be later discarded. However, in countries that allow paid donation some people are paid, and in some cases there are incentives other than money such as paid time off from work. People can also have blood drawn for their own future use (autologous donation). Donating is relatively safe, but some donors have bruising where the needle is inserted or may feel faint.
Potential donors are evaluated for anything that might make their blood unsafe to use. The screening includes testing for diseases that can be transmitted by a blood transfusion, including HIV and viral hepatitis. The donor must also answer questions about medical history and take a short physical examination to make sure the donation is not hazardous to his or her health. How often a donor can donate varies from days to months based on what component they donate and the laws of the country where the donation takes place. For example, in the United States, donors must wait 56 days (eight weeks) between whole-blood donations but only seven days between platelet apheresis donations and twice per seven-day period in plasma pheresis.
The amount of blood drawn and the methods vary. The collection can be done manually or with automated equipment that takes only specific components of the blood. Most of the components of blood used for transfusions have a short shelf life, and maintaining a constant supply is a persistent problem. This has led to some increased interest in auto transfusion, whereby a patient's blood is salvaged during surgery for continuous reinfusion—or alternatively, is "self-donated" prior to when it will be needed. (Generally, the notion of "donation" does not refer to giving to one's self, though in this context it has become somewhat acceptably idiomatic).
Provided and translated by : Javad Eynaki Maleki